As Shakespeare might have put it had he lived in 2023 amid the record-breaking heatwave that has gripped parts of Eastern Asia, Europe, and North America, “Now is the summer of our discontent”. Or, as Glenn Frye, founding member of the Eagles, famously voiced, “The Heat Is On”. And, right now, judging by how uncomfortable it feels outside, the heat is most definitely on.
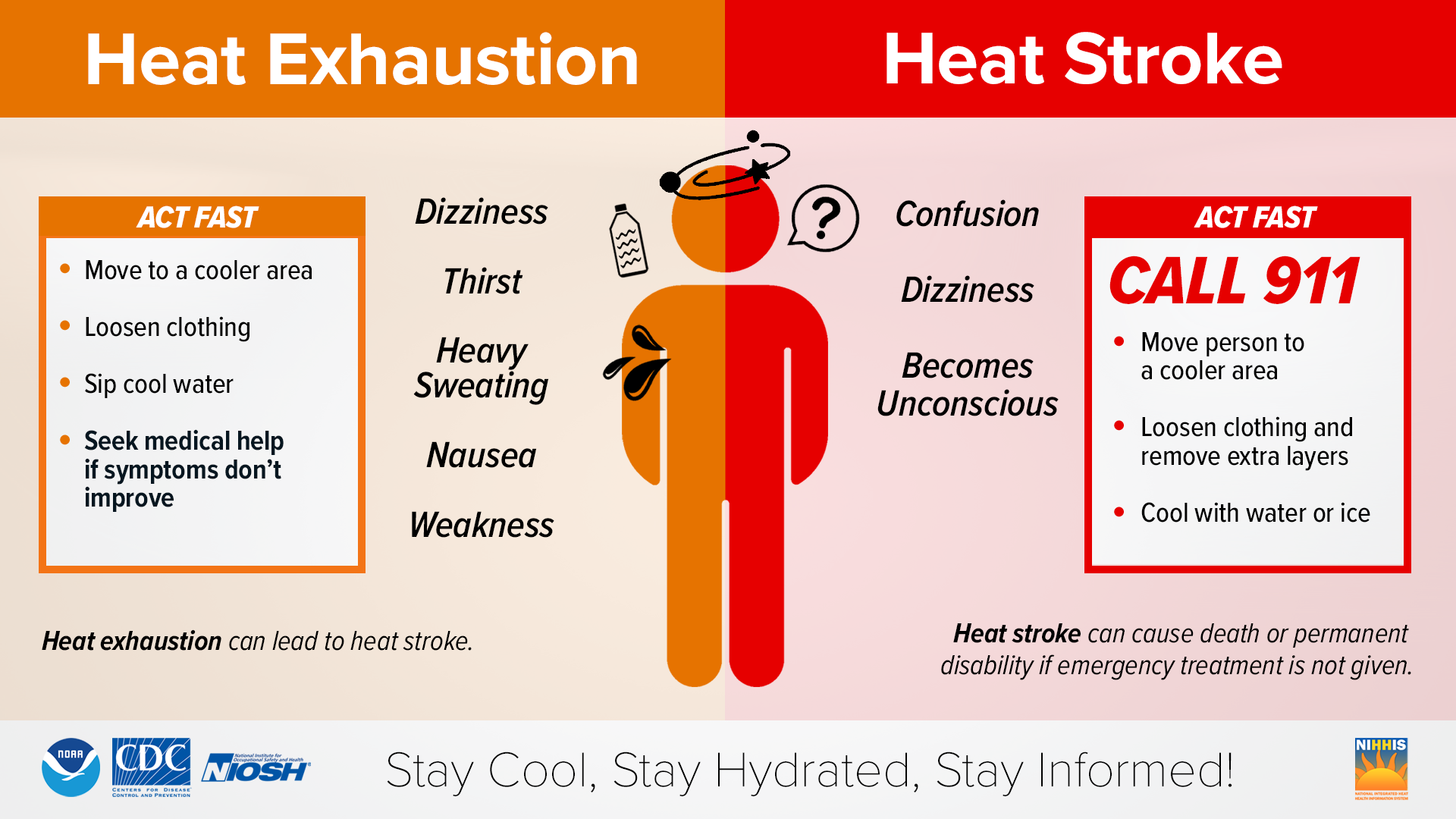
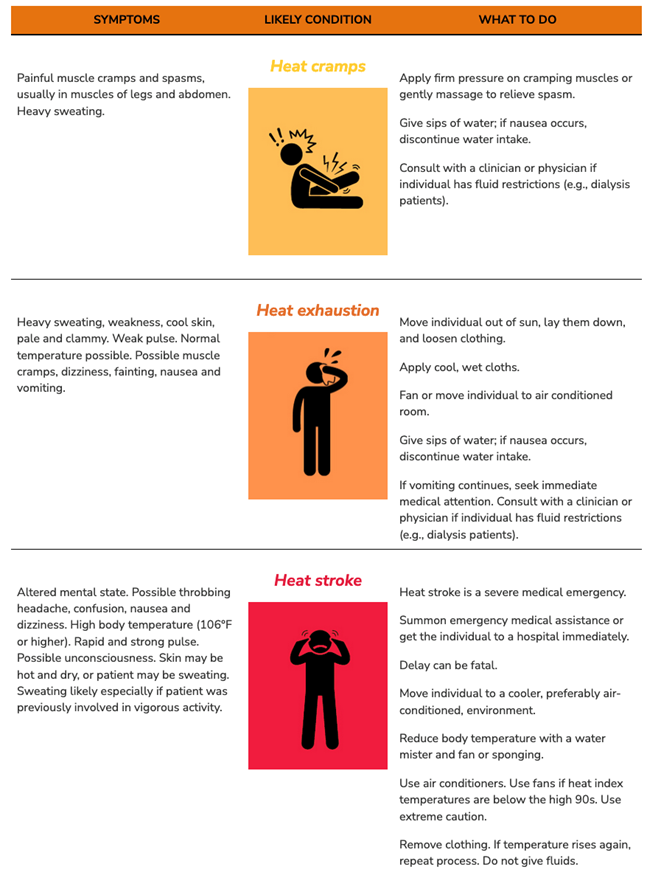
Once the temperature reaches or exceeds 35°C/95°F, the likelihood of heat illness or hyperthermia increases. Hyperthermia exists on a continuum ranging from minor heat stress (heat rash, cramps, etc.) to moderate heat exhaustion, the signs, and symptoms of which include intense thirst, weakness, discomfort, anxiety, dizziness, fainting and headache, and, finally, to life-threatening heat stroke where the core body temperature exceeds 40°C and nervous system dysfunction such as delirium, convulsions, or coma is present from direct damage to brain tissue.
Below is a graphic from the CDC, which lists the signs and symptoms of heat exhaustion and heatstroke and what to do if they are detected.
Most at risk for heat-related illnesses are the very young, the very old, and those with underlying diseases like diabetes, heart failure, chronic obstructive pulmonary disease (COPD), and Parkinson’s (PD) and related disorders like Lewy body dementia. This post specifically concerns itself with PD-related hyperthermia.
PD predisposes to hyperthermia because of 1) mobility problems, which may make it harder to increase fluid intake or to escape from hot environments, 2) sweating abnormalities, which compromise evaporative heat loss 3) use of anticholinergic medications such as trihexyphenidyl hydrochloride, procyclidine hydrochloride, diphenhydramine hydrochloride, and benztropine mesylate or antidepressants with anticholinergic activity that further decrease sweating and 4) susceptibility to pneumonia and urinary tract infections (UTIs).
Best preventative practices for PD patients (and other vulnerable populations like the elderly and those with underlying health conditions) are to:
- pay close attention to heat advisories or warnings
- shelter in cool indoor places, preferably with fans or air-conditioning, on hot summer days
- wear light-colored, loose-fitting lightweight clothing
- drink plenty of non-alcoholic and caffeine-free fluids
- use lukewarm baths or cold compresses to cool off, if possible
- consider discontinuation or dose reduction of anticholinergics and antidepressants with anticholinergic activity, if possible
- seek immediate medical attention for symptoms of heat illness
The warning signs and what to do for heat related illness are shown below in this graphic excerpted from the Excessive Heat Events Guidebook, Environmental Protection Agency.
Routine antibiotics are not indicated although infection should be ruled out. Antipyretics like acetaminophen (Tylenol) are not effective since hyperthermia is not the same as fever. The point at which to halt cooling is not well-defined, but a rectal temperature of 39°C is generally accepted and probably safe.
